
Placebo discovery could change how clinical trials operate
pharmafile | October 28, 2016 | News story | Medical Communications | Northwestern Medicine, Rehabilitation Institute of Chicago, brain, fMRI, pain relief
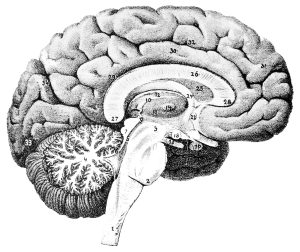
Researchers from Northwestern Medicine and the Rehabilitation Institute of Chicago (RIC) have pinpointed, for the first time, exactly which region of the brain is responsible for producing the ‘placebo effect’ in pain relief. The results of the study emerged from the use of fMRI technology that found the area, called the mid-frontal gyrus, had more connections with other parts of the brain in those that responded strongly to the placebo effect. The area plays a central role in our emotions and decision making.
The study used 95 patients who suffered from chronic pain associated with osteoarthritis, with researchers finding that around half of the participants possessed these mid-frontal gyrus that were likely to respond strongly to placebos. The study was based over two trials: one portion identified the active region related to susceptibility to the placebo effect that was then corroborated in the second clinical trial. The rate of success in identifying potential responders to placebos was at 95% in the second part of the trial.
The consequence of the study is the potential to design more ‘personalised’ pain relief to individuals. There are those, for instance, who do not respond to certain drugs and this report may provide answers as to why. Pain killing drug Lyrica (pregabalin), for instance, does not prove an effective treatment for all patients.
“If future similar studies can further expand and eventually provide a brain-based predictive best-therapy option for individual patients, it would dramatically decrease unnecessary exposure of patients to ineffective therapies and decrease the duration and magnitude of pain suffering and opioid use”, Marwan Baliki, research scientist at RIC, and Vania Apkarian, professor of physiology at Feinberg in whose lab the research was conducted, said.
If such ‘brain-based’ option were to be developed in the future, it would also allow clinical trials to be more selective in the patients that they choose to participate within studies. They could choose to eliminate those that have a particularly high response to placebos, allowing pain killing medication to be tested without interference from those who are particularly responsive to placebos.
Ben Hargreaves
Related Content

CBD could be used to deliver drugs into the brain, research shows
Cannabidiol (CBD), one of 113 cannabinoids in cannabis plants, could be used to deliver medicines …
Drug slows brain shrinkage associated with progressive multiple sclerosis, study shows
The multiple sclerosis drug ibudilast, slowed brain shrinkages in patients with progressive MS, a study …
US biotech company to try resurrect the clinically dead
A US biotech firm has announced plans for a Phase I trial that will see …






