
Breakthrough in personalised medicine as cancer vaccine shows results
pharmafile | July 6, 2017 | News story | Research and Development | Precision Medicine, personalised medicine, precision oncology
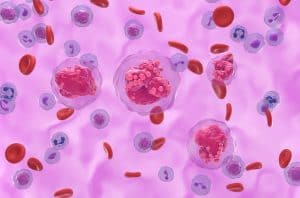
The old adage that everyone is unique holds a lot of water when it comes to cancer treatment. Research has found that tumours tend to be distinctive to an individual, with their own specific mutations and profile. It is for this reason that even immunotherapies, such as the PD-1/PD-L1 wave of treatments, are incredibly important, but they do not necessarily work for everyone.
In a sign of a treatment that may emerge as part of a new raft of targeted treatment for cancer, early studies have shown that a ‘cancer vaccine’ may be a feasible therapeutic method in the future.
The neoantigen vaccines were unique to the patients in the trials, with scientists sequencing tumour cells to discover the particular mutations that are not evident in healthy cells. The researchers then identified the antigens that immune cells are likely to target before dosing the patients with millions of copies of between 13 and 20 different antigens.
The theory behind the research is that the body would then recognise the antigens as a foreign substance in the body and respond with the immune system. Once an immune response has been learned, to attack the particular antigen associated with the tumour cells, it could then begin to attack and destroy the tumour cells themselves.
In the clinical trials set up to test this theory, this is almost exactly how the research panned out. In the larger of the two trials, eight of 13 melanoma patients were in complete remission two years after taking the vaccine created for them. Of the five patients who did not respond, objective responses were recorded and another patient showed positive results in combination with a PD-1 immunotherapy. In the smaller study, four of the six patients were found to be cancer-free after two years.
“This research shows that it is feasible to produce peptide-based personalized neoantigen vaccines, and these vaccines can generate immune responses with reliability and potency,” said Catherine Wu, who led the smaller of the two studies. “In this study, over 70% of all peptides successfully generated measurable CD4 and/or CD8 T cell responses. In addition, while patient numbers are limited, the initial clinical data is intriguing and worthy of exploration beyond the adjuvant setting into patients with active disease with immuno-oncology combinations.”
The main drawback of such a treatment is that it requires each patient to have their tumour cells sequenced, which is a time-consuming and expensive process. The treatment would cost around six figures and the treatment would be generated within two months but both of these figures are expected to drop. As sequencing DNA becomes more advanced, it should see a reduction in time and price.
One particular weakness that was discovered in the treatment method itself is that not everyone has enough mutations within tumour cells to effectively target them – potentially limiting who could benefit from the treatment. Beyond this, the trials were also conducted without control arms so it is difficult to say whether the results exhibited would not have happened in standard treatment. The next stage is to take the method of treatment into larger scale studies.
Ben Hargreaves
Related Content
AI-powered prognosis test company Spotlight Medical secures €6.2m in seed funding
Start-up Spotlight Medical has announced it has raised €6.2m in a seed funding round led by …

Breakthrough announced in circulating tumour cell research
Liquid biopsy company, Angle, has announced results from their study in non-small cell lung cancer …

University of Glasgow research details promising precision medicine approach in pancreatic cancer
Researchers at the University of Glasgow have unveiled a new precision medicine approach to identify …






