
Tangles and plaques: unlocking the secrets of Alzheimer’s disease
pharmafile | March 11, 2011 | Feature | Research and Development, Sales and Marketing | Alzheimer's, Alzheimer's disease, bapineuzumab, dimebon, latrepirdine, solanezumab
Despite many years of relentless research efforts, Alzheimer’s disease, the most common form of dementia, remains impossible to cure.
According to Alzheimer’s Disease International, 35.6 million people have the disease worldwide, but the number of sufferers is expected to triple by 2050. This will create a huge burden on unpaid carers and health and social care systems.
There are currently no drugs available that can stop or reverse the relentless march of Alzheimer’s disease. Of all the new therapies that have been investigated in the last ten years, more than 20 have failed late-stage clinical trials. But now, for the first time, three potential Alzheimer’s treatments are in phase III – so are we close to a breakthrough, or at least a step forward in fighting the disease?
Beyond cholinesterase inhibitors
Acetylcholinesterase inhibitors (AChEIs) are the current standard treatment, and help maintain levels of acetylcholine in the brain, which is essential to ensure the proper functioning of memory and cognition. They do so by preventing the breakdown of acetylcholine by the enzyme acethylcholinesterase.
There are three cholinesterase inhibitors on the market – Novartis’ Exelon (rivastigmine), Janssen and Shire’s Reminyl (galantamine) and Eisai and Pfizer’s market leader Aricept (donepezil).
The drugs can improve the symptoms, and delay the progression of Alzheimer’s disease, but they cannot halt or reverse its course.
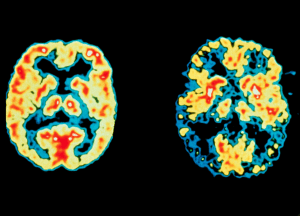
The past few years have seen a surge of clinical trials of new Alzheimer’s drugs. These differ from existing treatments, as they target the likely cause of Alzheimer’s, rather than its symptoms. Researchers noticed that the brains of Alzheimer’s sufferers were distinguished by two distinct features – ‘plaques’ and ‘tangles’ in certain parts of the brain. It emerged that the plaques are deposits of the protein beta-amyloid (Aβ) that form outside nerve cells. The tangles are thread-like structures of the protein tau and form inside nerve cells. Most of the work in the last 20 years has centred around understanding the role of these two phenomena in causing the disease, in the assumption that they play a direct role.
The ‘Amyloid Hypothesis’ was first put forward in 1991, suggesting that Alzheimer’s disease is triggered by its action, and numerous drugs have sought to halt this process by increasing the removal of excess beta-amyloid from the brain, by reducing the protein’s production, or by preventing it from clumping into plaques.
Late-stage failures
Many drugs which have been designed to target beta amyloid have failed. Lilly’s semagacestat is one of the latest – the company announced it would end its clinical development in August 2010, following results from two phase III trials on patients with mild or moderate AD.
To the dismay of researchers, the trial showed that semagacestat actually accelerated the progression of the disease instead of slowing it down. The drug also led to a significant decline in physical and mental functioning, and increased the risk of skin cancer.
Semagacestat belongs to a class of drugs called gamma secretase inhibitors, which block the enzyme involved in the production of beta-amyloid molecules from its larger precursor protein, known as APP (amyloid precursor protein).
In 2008, another gamma secretase inhibitor, Myriad Genetics’ tarenflurbil was found ineffective at improving both the cognitive function and the ability to perform simple activities of daily living, such as dressing and eating, in patients with mild Alzheimer’s disease.
Similarly disappointing results had been obtained previously for Neurochem’s Alzhemed (tramiprosate). Alzhemed has yet another mechanism of action, binding to beta-amyloid molecules and thereby stopping them from clumping together into plaques.
These failures have cast doubt on the amyloid hypothesis, as there is no conclusive evidence that accumulation of beta-amyloid in the brain is the primary cause of Alzheimer’s disease.
Few doubt that beta-amyloid is somehow tied up with Alzheimer’s, but it is now clear the pathology is far more complex than first hoped.
According to Steven Paul, former head of Science and Technology at Lilly and president of Lilly Research Laboratories, the amyloid hypothesis isn’t wrong, but rather the new agents are being tested on the wrong patients.
Most phase III trials involve patients with mild or moderate AD. Paul says, the brain is too damaged to be rescued by anti-beta-amyloid drugs by this stage. For this reason, trials should involve patients earlier in the course of the disease.
Writing in the journal Nature, Paul points out: “It’s now clear that Aβ is building up and depositing in the brain a full decade or more before you even get mild cognitive impairment, which is considered to be the prodromal state of Alzheimer’s disease.
“In my opinion, a good test for the hypothesis – especially with secretase inhibitors that decrease Aβ synthesis – would require treating patients very early in the disease, or even those who are asymptomatic.”
The tau hypothesis
A rival theory is the tau hypothesis. This has gained ground as evidence has failed to emerge showing a direct link between amyloid and the loss of neurons in the brain. Researchers now think the built up of tau in the brain proves to be toxic for cells, and causes them to die. The theory is further supported by similar disease known as tauopathies, in which the same protein is identifiably misfolded.
Closing in on the pathology
In December, new research was published which could represent a subtle but significant advance in our understanding of the disease. Randall Bateman, MD, an assistant professor of neurology at Washington University in St. Louis tested his hypothesis that Alzheimer’s sufferers produce normal amounts of beta-amyloid, but that it is not cleared or removed efficiently from the brain as it is normally.
The finding should help advance understanding of what pathways are most important in the development of Alzheimer’s pathology, and may one day lead to an improved biomarker to help provide earlier diagnosis as well as new treatments.
Dr. Bateman and his researchers used a study of cerebrospinal fluid (CSF) to measure beta-amyloid production, and clearance rates in study volunteers with Alzheimer’s disease and in age-matched volunteers free of the disease.
‘‘This study is significant in that it reports the first measurement of beta-amyloid production and clearance in Alzheimer’s,” said Marcelle Morrison-Bogorad, PhD, director of the Division of Neuroscience at the National Institute on Aging (NIA).
‘‘For years scientists believed that it was the overproduction of beta-amyloid that led to its accumulation in the brain. These new findings shift the emphasis to clearance of beta-amyloid. This may lead to development of a diagnostic test as well as identification of new therapeutic targets.”
Late-stage survivors
There are presently three disease-modifying drugs in phase III trials which could reach patients within the next few years. Lilly and Elan’s anti-beta-amyloid monoclonal antibody, solanezumab, is expected to complete phase III trials in April 2012.
Solanezumab binds specifically to soluble amyloid beta, and thereby may draw the peptide away from the brain through the blood. In earlier short-term clinical studies, solanezumab appeared to have dose-dependent effects on amyloid beta in blood and cerebrospinal fluid.
But these studies were too short to evaluate any potential delay in the progress of Alzheimer’s disease, something which Lilly hopes the phase III trials will provide.
Next is Pfizer/Medivation’s Dimebon (latrepirdine), a mitochondrial function modulator for use in severe Alzheimer’s.
Dimebon protects nerve cells in the brain against damage and death by ensuring the good functioning of their mitochondria, the cell’s energy centre. Medivation completed patient enrolment in November 2010 in the CONCERT study – a 12-month, phase III clinical trial in patients with mild-to-moderate Alzheimer’s evaluating the potential efficacy of Dimebon when added to ongoing treatment with Aricept (donepezil).
Top-line results from the CONCERT trial are expected in the first half of 2012. The FDA has confirmed that the company can use its phase III CONCERT trial to complete the registration package for mild-to-moderate Alzheimer’s disease, provided that the results are robustly positive.
Finally, there is bapineuzumab, being co-developed by Johnson & Johnson and Pfizer.
Bapineuzumab is an anti-beta-amyloid humanised monoclonal antibody. It binds to beta-amyloid molecules and removes them from the brain. This in turn prevents the formation of plaques, which, as we have seen, are considered central to the development and progression of the disease.
A study published last year in The Lancet found that in patients with mild or moderate Alzheimer’s disease, treatment with bapineuzumab reduced beta-amyloid in the brain by 25 per cent.
Subsequent research also showed that bapineuzumab lowers brain levels of the tau protein, giving it a second potential avenue for treating the disease. This could give the drug two opportunities to help Alzheimer’s patients.
Kaj Blennow, MD, PhD, of the University of Gothenburg, Sweden is the lead investigator at one of the global sites investigating bapineuzumab.
‘‘These observations suggest that immunotherapy treatment targeting amyloid may also alter neurodegenerative processes that occur later in the disease process and that are more directly associated with loss of function,” Blennow said. ‘‘However, this was a small study and these findings need to be confirmed.”
There are many more candidates currently in earlier clinical and pre-clinical development, but information about different mechanisms being studied is in short supply. Roche, the current leader in oncology is trying to expand its portfolio into CNS drugs, and has two drugs in phase II being studied for Alzheimer’s, (RG3487 and RG1450) and RG1662 for ‘cognitive disorders’, with a further Alzheimer’s candidate in phase I.
Genenetech, Roche’s standalone biotech arm also has an anti-beta-amyloid treatment in phase II.
Not the ‘magic bullet’
After so many disappointments, experts are careful not to be too bullish about these phase III hopefuls being a great step forward in treatment.
Professor John Hardy is professor of neuroscience and chair of molecular biology for neurological disease at University College London, and is credited as one of the originators of the amyloid hypothesis in the 1990s.
He says: “The answer to these questions depend primarily on whether or not there will be definite proof that the drugs under development actually work. Should this happen, it would be a major step forward compared to cholinesterase inhibitors, which only treat the symptoms of the disease.”
At present, however, he says many doubt that any of the drugs in the pipeline could represent an advance in treatment. “I think there is some pessimism that anything is ever going to change substantially for patients,” says Hardy.
“We all hoped that the results from the clinical trials on the new agents would show that these were going to be the ultimate therapy for Alzheimer’s disease” – only time will tell if this is the case or not.
Looking ahead, Hardy thinks any successfully launched new treatment will not instantly replace the current standard of treatment.
“The likely future scenario is that cholinesterase inhibitors will continue to be the drugs of choice for patients with Alzheimer’s disease, and investigational drugs will be used as adjunctive therapies – if proven effective. We are moving from the idea of a ‘magic bullet’ to the idea of polypharmacy, whereby different drugs will likely be used simultaneously, each one of which will make a small, but significant, difference in the patients’ lives.”
This is true for the majority of medical conditions, where the goal is to ensure the maximum benefit to patients. Hardy says: “Take type II diabetes, for instance. People with this condition are given insulin, which targets the cause of their condition. But they also take statins, which help reduce their hypercholesterolemia, one of the symptoms of their condition.”
Something similar will be possible for Alzheimer’s patients in the years to come.
Yet, whether or not the current phase III candidates prove to be successful, research must continue to fight the devastating effects of Alzheimer’s and its growing incidence around the world.
A ROLE FOR DIABETES DRUGS?
New research suggests that new diabetes drugs enhance cell growth in the brain, and could help treat Alzheimer’s disease.
Researchers at the University of Ulster in Coleraine funded by research charity the Alzheimer’s Research Trust, studied the effects of two drugs – Novo Nordisk’s Victoza (liraglutide) and Lilly’s Byetta (exenatide) – as part of an investigation into the link between diabetes and Alzheimer’s disease.
The drugs mimic a hormone called GLP-1, which helps the body produce insulin. But the team at Ulster, led by Dr Christian Hölscher, found that in mice with diabetes, the drugs also stimulated the growth of new brain cells.
They now hope their findings, published in the Journal of Neuroscience Research, could help scientists in the search for a potential treatment for Alzheimer’s.
Further research by the same team found that in mice with Alzheimer’s, liraglutide enhanced brain cell growth and reduced the build-up of a protein called amyloid in the brain – a key feature of the disease – as well as protecting the formation of memories.
Dr Hölscher, who presented his latest findings at the prestigious Society for Neurosciences annual meeting, said: “It has been known for some time that diabetes is a risk factor for developing Alzheimer’s disease, and we know that in diabetes, the growth and replacement of cells in the brain are compromised, putting the brain at risk of further damage.
“We are very excited about our results, which show that these drugs are able to enter the brain, where they can help protect and replace cells. Because the drugs are already approved for use in people, this is a rich field for future research, and we would now like to see clinical trials to test the effects of these drugs in people with Alzheimer’s.”
Related Content

Sanofi completes acquisition of Vigil Neuroscience to early neurology pipeline
Sanofi has announced that it has finalised its acquisition of Vigil Neuroscience, a US-based biotechnology …
Lilly’s drug for early Alzheimer’s shows promising results
Eli Lilly (Lilly) has announced positive new data from the long-term extension of its phase …
Roche receives CE Mark for blood test to help rule out Alzheimer’s
Roche has been granted CE Mark approval for its Elecsys pTau181 test, the first in …






