The case for adaptive trials in dementia
pharmafile | January 6, 2016 | Feature | Manufacturing and Production, Research and Development | Alzheimer's, Alzheimer's disease, adaptive trials, research
An ageing population and widespread chronic neuro-degenerative disease will make dementia an ever increasing burden on society, families and the individual while also offering an unprecedented opportunity for new drugs to be taken to market.
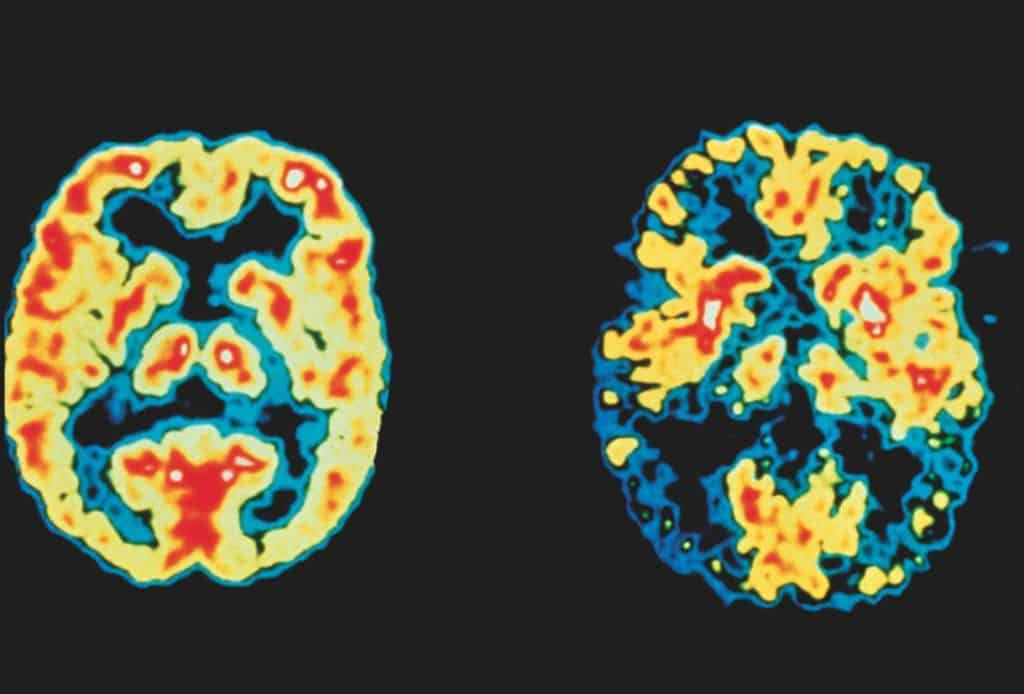
Despite dedicated efforts over many years, we still lack full understanding of the disease course, and have little to offer in the way of treatments. Alzheimer’s disease, the most prevalent cause of dementia, is brutally progressive, has no cure, and places tremendous burden on our healthcare system, carers, and families.
Currently in the UK we treat Alzheimer’s disease using treatments that help manage symptoms, but are unable to fully cure the disease or prevent its progress.
We are now able to identify signs of Alzheimer’s disease in the brain many years before early symptoms appear. This discovery has led to increasing focus by researchers to find ways to stop the disease during the pre-symptomatic phase, which could delay the onset of symptoms, or even prevent them from appearing at all.
This line of research presents many challenges. Our knowledge of dementia is as yet not as advanced as our knowledge of other major conditions, such as heart disease. Identifying candidates who are likely to develop the disease can be problematic, and traditional methodologies used by most research companies are notoriously inflexible, often leading to high attrition rates, lengthy development programs and increasing development costs. Two innovations are emerging that may address some of these challenges.
Making the case
The case for using adaptive trials as a methodology to research dementia is strong. They are known to improve trial efficiency, adding value to all phases of development. In exploratory phases of drug development, adaptive trials can combine development phases and improve resource allocation. In confirmatory trials they enable early stopping, change of allocation rates and reassessment of the sample size, patient subgroups or specific treatment arms.
By testing candidate drugs in parallel during the adaptive trials process, a greater number of candidates could benefit from a suitable active treatment. New drugs can be trialed and stopped if found ineffective, reducing waste and reducing the suffering of a participant trialing a treatment that does not work for them. Both individual drugs and combinations of medicines can be tested, allowing participants to experience the best options available to them while also increasing efficiency by reusing protocols, staff and infrastructure across a number of compounds.
Trials can also be adapted in response to initial results, offering more successful treatments to a wider group to test findings if certain traits shared by groups are discovered. This enables researchers to see trends and similarities amongst candidates who respond better to different medicines, which in turn will allow healthcare professionals to offer a more tailored treatment to individuals with similar backgrounds.
Potential benefits
With better data and improved decision-making, adaptive trials can increase the probability of success and decrease development time. Advanced analytics are required, as is investment in probabilistic models of disease progression and trial simulation, to understand potential information gain if participants are deployed to different arms of the trial. It may be possible to pool placebo cases, which yields additional efficiency.
Adaptive trials have a critical role to play in delivering increased product development efficiency and productivity in the pharmaceutical sector. While it is apparent adaptive trials can be highly beneficial in the search for a cure for dementia, the large volume of data generated by these types of trials, from large and varied groups, must be carefully monitored. To facilitate fast and transparent communication between the trials, a cloud-based informatics platform is required to focus on the technical challenges of defining a repeatable model for running adaptive trials particularly suited for pre-competitive consortia.
Current research projects
The European Prevention of Alzheimer’s Dementia (EPAD) programme from the Innovative Medicines Initiative (IMI) will use this adaptive trialling method to test Alzheimer’s dementia prevention treatments while the disease is in the pre-symptomatic phase.
The project, jointly funded by the EU and the European Federation of Pharmaceutical Industries and Associations (EFPIA), has created its own register, identifying 24,000 people across Europe who may be at risk of developing the disease. Those deemed at ‘high risk’ will undergo standardised tests, and will then be considered for selection to take part in EPAD’s adaptive trials process on proof of concept trials.
Today there is a growing social trend for people wanting more of a stake in their healthcare and being able to manage the level of information they get. Additionally trial recruitment is often a challenge and estimates of participation often turn out to be overly optimistic. Privacy continues to be a factor, with new EU legislation requiring specific consent.
While this prospect is daunting for traditional research groups, organisations can ‘grasp the nettle’ by implementing a system of dynamic consent and working with patient organisations to establish trust and reliable participation.
Gaining patient engagement
Research groups can address these challenges by applying a participant-focused approach to consent, the dynamic consent model. Patients are given the opportunity to control the flow of data at the level of consent and can opt out of giving access to specific projects. For example, they might wish to allow academic researchers studying genetics to use their data, but not a nutritional expert or a neurosurgeon.
They can also audit their information usage, choose their preferred method of contact, and change their privacy settings. Being able to see one’s outcome is important too – finding out if my data or sample led to anything useful, interesting or personally important. By giving patients better control of their data, their confidence in participating in research is enhanced, and they are more likely to agree to undertake the project.
The increase of patients agreeing to participate in dementia research is critical. Our healthcare system is already under immense strain, and the projected additional care and pharmaceutical requirements for dementia sufferers must be addressed immediately to prepare our communities to cope with this burden.
What needs to happen next
Adaptive trials bolstered by the dynamic consent model will allow this important research to be undertaken quickly, and will help reach a greater number of patients at the earliest opportunity. Combining these two techniques will require the implementation of IT architectures that span public, corporate and healthcare networks.
By using a safe and transparent data system, we can advance dementia patient care, giving us the ability to better identify the most effective care pathways for patients, and dramatically improve care management – with less risky and more profitable research and development.
Rodrigo Barnes is chief technology officer at Aridhia.
Related Content

FDA accepts Eisai’s Leqembi sBLA for early AD treatment
Eisai and Biogen have announced that the US Food and Drug Administration (FDA) has accepted …

Nxera Pharma partner Neurocrine Biosciences enters phase 1 NBI-1117567 study
Nxera Pharma’s neuroscience-focused biopharmaceutical partner Neurocrine Biosciences has announced it has successfully started its phase …

Bayer and Aignostics to collaborate for AI oncology research
Bayer and Aignostics have announced that they have entered into a strategic collaboration for several …